Drug Alerts
 Drug alerts advise our community about potential substances that could put individuals at risks or cause harm. They are shared with service and health care providers, community partners, harm reduction sites, and the public to warn that there are dangerous substances in the community that have been associated with increases in overdoses and poisoning.
Drug alerts advise our community about potential substances that could put individuals at risks or cause harm. They are shared with service and health care providers, community partners, harm reduction sites, and the public to warn that there are dangerous substances in the community that have been associated with increases in overdoses and poisoning.
Staying informed helps our community stay healthy and safe. Northeastern Public Health (NEPH) will share all available information such as the as name, description and effects of the drug.
When a alert is issued, NEPH will also increase harm reduction messaging and resources, with information on responding to an overdose, tips for safer dug use, the Good Samaritan Law, where to get naloxone, and where to get harm reduction supplies.
|
|
|
Alerts inform of increased opioid-related incidents
(overdose, poisonings, hospitalizations, deaths) events in the area.
AND/OR
Inform of new, synthetic, high dosage, or toxic drug supply in the area and neighbouring districts.
|
Past and current alerts
Report Bad Drugs in Timiskaming
If you or someone you know had a bad reaction to street drugs, including if you experienced an overdose, you can make an anonymous report about it to Northeastern Public Health. This site is checked regularly for new reports.
You do not have to answer all the questions, but please include as much detail as you can. Please DO NOT include names or other identifying information in any of the comments.
You can make one report at a time to tell people about:
- An overdose caused by street drugs, including opioids such as fentanyl, morphine etc.
- An unexpected or bad reaction to drugs
- Other concerns for your community related to drug overdose or other harms
For more information, please see the Report Bad Drugs Q&A.
The information submitted will be reviewed and used to inform actions within the community. If you have any questions about this reporting, please contact us.
What Is Xylazine?
- Xylazine is a tranquilizer used in veterinary medicine. It has analgesic and muscle relaxant properties.
- It requires a veterinary licence for purchase and use. Trade names include Rompun® and Anased®.
- It is not approved for human use by any authorizing association in Canada nor the United States.
Xylazine in the Unregulated Drug Supply:
- Xylazine use among people who use drugs has been reported in the literature since the early 2000s. It was first identified in the unregulated drug supply in Canada in 2012.
- There is evidence for both intentional and unintentional use of xylazine. For example, people who use drugs have reported using it to prolong some of the effects of fentanyl.
- It has also emerged as an increasingly common cutting agent in both Canada and the United States. It is commonly added to opioids on the unregulated market, particularly fentanyl, and has also been identified alongside cocaine and methamphetamine.
Why Is It a Concern?
- Xylazine can lower heart rate, blood pressure and breathing. Combining xylazine with opioids or central nervous system depressants like benzodiazepines or alcohol can significantly depress these vital functions, increasing the risk of overdose and death.
- Because xylazine is sometimes added to opioids as an adulterant, people may be unaware of its presence in the unregulated supply, raising the risk for people who use drugs.
- For overdoses involving combinations of xylazine and opioids, naloxone can reverse the opioid effects but has no effect on xylazine. This can impact the success of the overdose response. There is no pharmaceutical antidote specifically for xylazine.
- Frequent xylazine use is reportedly associated with a higher prevalence of skin problems, including abscesses, ulcers and infections (compared with those who do not use xylazine).
Let’s Talk Xylazine - Information for Harm Reduction Workers (CATIE)
Naloxone saves lives!
Recognize the signs of an overdose and know what to do. Learn how and when to use naloxone - Naloxone (pronounced na-LOX-own) is a fast-acting drug used to temporarily reverse the effects of opioid overdoses.
If you or someone you know is using opioids, make sure to carry naloxone with you. It’s free, available without a prescription and can be picked up at most pharmacies or at Northeaster Public Health.
Preventing and responding to an overdose and naloxone
Anything can be cut with fentanyl or carfentanil. There is no way to be sure of what is exactly in drugs obtained from anywhere other than a pharmacy or government retailer (such as an Ontario Cannabis Store). If you get them from a friend, order them online, buy them from a dealer, or anywhere similar, you don’t know how toxic they may be.
Counterfeit pills can be made to look almost identical to prescription opioids and other medications. Illicit fentanyl is often made as a powder and mixed with other drugs (like heroin, cocaine or crack). It can also be pressed into pills and sold as 'oxycodone' (OxyContin, oxys, Percocet, percs, 80s) or other pills, including speed and ecstasy/MDMA.
There is no easy way to know if fentanyl is in the drugs you are using. You can't see it, smell it or taste it. A very small amount of the powder can cause an overdose.
How to reduce your risk
If you use opioids, you can reduce your risk of overdose death by:
Not using alone
- When using with someone else, don't use at the same time. Be sure your friend is willing to call for help and make a plan for what to do if an overdose happens.
- If you do use alone, tell someone before you use. Have a safety plan, leave the door unlocked and have someone come check on you. You can also call the National Overdose Prevention Line at 1-888-688-NORS (6677) or connect with an anonymous virtual harm reduction supporter via the Brave App.
Don't mix drugs
Don't mix drugs with other drugs or alcohol. Mixing puts you at higher risk of overdose.
- Use one drug at a time or if you plan on mixing, use less of each drug.
Go slow
The quality of illicit drugs is unpredictable. Fentanyl is being cut (mixed) into both opioid and non-opioid drugs like powder and mixed into cocaine, heroin, and crack or like pills and being sold as 'oxycodone' (80s, oxys) or other pills including ecstasy/MDMA.
- Use in small amounts and do "testers" (or test doses) to check the strength of what you are using, but know that a small amount can cause an overdose.
Carry naloxone
Naloxone is a medication that can temporarily reverse the effects of an opioid overdose. Naloxone is available free to persons who use drugs and their family and friends!
Know your tolerance
Tolerance is the body's ability to handle the effects of the drug being used. Tolerance to a drug develops over time.
Drug tolerance will decrease when somebody has taken a break from using - whether intentionally or unintentionally (for example, while in treatment, at the hospital or in jail). Your tolerance will also change depending on:
- Weight
- Illness
- Stress
- Lower immune system (from hepatitis for example)
- Lack of sleep
- Other drugs/medications being used
- General health.
Use less drugs when your tolerance may be lower.
Your risk of overdose increases if you are new to using drugs or haven't used in a while!
Be aware
Drugs can be tampered with at any point. People selling drugs may not be aware if it has been mixed with anything before they sell it to you.
Signs and symptoms of an overdose
|
Type of drug
|
Common signs and symptoms of an overdose
|
|
Opioids
(Examples like heroin, morphine, fentanyl, methadone, OxyContin
|
Breathing is very slow, or irregular,
or they may not be breathing at all
Fingernails and/or lips are blue
Body is limp
Deep snoring or gurgling sounds
Loss of consciousness/passed out (can't wake the person up)
Unresponsive (not answering when you talk to them or shake them)
Pinpoint (tiny) pupils
|
|
Stimulants
(Examples like cocaine, speed, crystal meth, MDMA/ecstasy)
|
Seizures
Pressure and tightness in chest
Foaming at the mouth
Racing pulse
Excessive sweating
Vomiting
Headaches/dizziness/ringing in the
ears
Hard time breathing
Sudden collapse
Loss of consciousness/passed out (can't wake the person up)
|
|
Hallucinogens
(Examples like acid, LSD, ketamine, magic mushrooms)
|
Catatonic syndrome (person will be in
a trancelike state)
Psychosis (their reality is altered
and may be having hallucinations or delusions)
Nausea/vomiting
Seizures
|
It is important to note that Naloxone is only effective with opioid overdoses.
How to respond to an opioid overdose
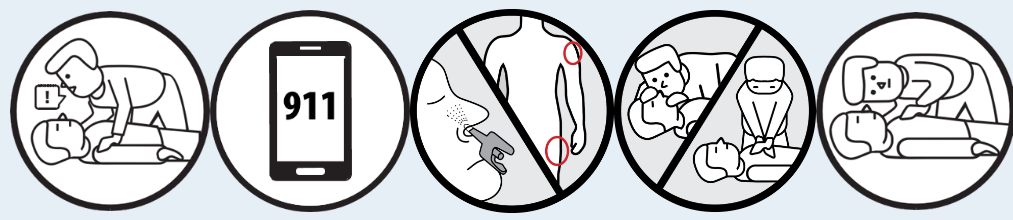
What to do in case of overdose
Remember to put on the non-latex gloves that come in your naloxone kit before you respond.
1. Shout the person’s name and shake their shoulders.
2. Call 9-1-1 right away if unresponsive.
3. Give naloxone:
- Spray: insert nozzle into nostril, then press plunger down firmly to give the dose (only spray once plunger is in the nostril)
Or
- Injectable: inject 1 vial or ampoule into arm or leg
4. Perform chest compressions only (not rescue breaths).
5. Is it working? If no improvement after 2-3 minutes, repeat steps 3 and 4.
6. Stay with them.
If the person begins breathing on their own, or if you have to leave the person at any time, put them in the recovery position. The recovery position helps keep a person's airway open so they can breathe and can prevent them from choking on vomit or spit.
Recovery Position
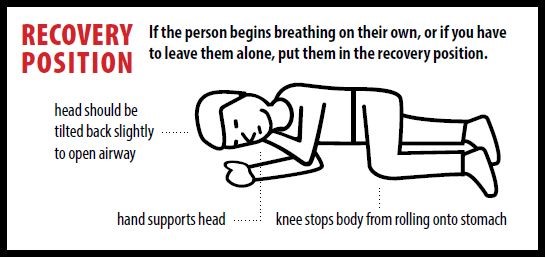
1. Responder extending victims closest arm above the victim’s head
2. Responder positions other arm across the victim's chest and bends furthest leg at the knee. Victim is rolled towards responder and placed on side
3. Victim laying on side with head stabilized on extended arm. Knee is bent and stabilized
It is important to stay with a person after giving them naloxone for the following reasons:
- The person may be confused and frightened when they wake up. You will need to tell them what happened.
- A lot of opioids can last longer in the body than naloxone, so an overdose could return. It is important to make sure that the person knows not to take any more drugs.
- It is important to tell paramedics everything you know about the situation so they can provide the best care.
- Naloxone may cause people who have used opioids to go into withdrawal. This may make the person want to use again. Using more will increase the risk of overdose as the naloxone wears off.
- Withdrawal can be very uncomfortable for the person but is not life threatening. Withdrawal symptoms may include:
- Muscle aches,
- Sweating,
- Nausea/vomiting,
- Agitation,
- Irritability.
Only opioids will respond to naloxone. Learn about tips on how to respond to overdoses of a stimulant (PDF) like cocaine, crystal meth, speed, MDMA, or Ritalin.
Naloxone and where to get a kit
An overdose is a life-threatening medical emergency. Naloxone is a medication that can temporarily reverse the effects of an opioid overdose, but it does not cure an overdose. If anyone suspects or witnesses a person experiencing a drug overdose, call 911 and administer naloxone, even if the drug consumed is unknown. Example of opioids include heroin, morphine, codeine, Percocet, methadone, fentanyl, carfentanil, etc.
Being able to recognize the signs of an overdose quickly and having a naloxone kit can save a life. Naloxone can buy time while paramedics are en route. Take-home naloxone kits do not replace the need for emergency care or minimize the importance of calling 911.
Effects of naloxone
In an opioid overdose, a person's breathing slows down or stops. Naloxone blocks the effect of opioids on the brain. It temporarily reverses these effects on a person's breathing. Giving naloxone can prevent death or brain damage from lack of oxygen.
Naloxone will only work on opioid-related overdoses. It is important to remember that a lot of other drugs are being mixed with fentanyl and carfentanil. If the person has used any drugs and is showing signs of an opioid overdose call 911 and give naloxone.
How long does naloxone take to work?
Once given, naloxone will start to work in approximately 2-3 minutes.
Naloxone stays active in the body for up to 2 hours but it is important to know that most opioids stay active in the body longer than 2 hours! If the opioid is still in the body after the naloxone wears off, the overdose can return!
- This is why it is so important to call 911 in every overdose situation!
Limitations
Giving naloxone to someone that is unconscious because of a non-opioid overdose is unlikely to cause more harm. Overdoses are life-threatening. Giving naloxone is better than not administering it.
The only reason to not give naloxone to someone who is experiencing an overdose is if the person is known to have a life-threatening allergy to naloxone or any of the ingredients. If allergies are unknown (which is likely the case when responding to medical emergencies), give naloxone.
Naloxone is safe for all ages. An opioid overdose is a life-threatening situation, which can be temporarily reversed by naloxone, and for that reason, naloxone can be given regardless of age, if the person is pregnant or lactating and if they have medical conditions such as heart, respiratory, liver or kidney disease.
For more information about using naloxone, see below:
Take-home naloxone kits
In Ontario, naloxone is available for free through local pharmacies and health unit offices. . It is available to persons who could be at risk of an overdose and to people who could help someone who is overdosing. When you get your kit, you will also receive training on overdose prevention, recognizing an overdose and how to respond.
Online Training
NaloxoneCare.com is an online learning portal to help individuals learn how to recognize the signs and symptoms of an opioid overdose and how to give naloxone. You can get a free nasal naloxone kit once the training is completed.
Good Samaritan Drug Overdose Act
The Good Samaritan Drug Overdose Act protects you, the person who is overdosing, and anyone at the scene from being charged with:
- Possession of controlled substances (example, drugs)
- Breaches in pre-trial release, probation orders, conditional sentences, or parole related to simple possession
The Good Samaritan Drug Overdose Act does not provide protection against charges for:
- Outstanding arrest warrants
- Making and selling of controlled substances (example, drugs)
- All other crimes not outlined within the Act
For more information, visit the Government of Canada website.
20251024/wh:tr
Report Bad Drugs